Originally published on 9th February 2021 Last updated on 7th August 2024
A ‘high-risk pregnancy’ is one of greater risk to the mother or her baby, compared to a more straightforward pregnancy.
Having hypothyroidism and/or Hashimoto’s are considered to be risk factors. [1]
High Risk Factors
Several factors can make a pregnancy high risk, including existing health conditions (such as thyroid disease) and health issues that happen before or during pregnancy.
- Pre-existing health conditions, such as: high blood pressure, PCOS, diabetes, kidney disease, autoimmune diseases, thyroid issues
- Obesity
- Drug/alcohol/cigarette use
- Age: teenagers, older mothers-to-be (35+)
- Twin, triplet+ pregnancies
- Having had a previous preterm birth
- Birth defects or genetic conditions in the baby
- Health conditions which develop during pregnancy, such as: preeclampsia, gestational diabetes, Low Papp-A, Abnormal liver function
So, We’re Classed as ‘High Risk’ then?
With ‘thyroid issues’ on the list, that covers hypothyroidism and Hashimoto’s, and with ‘autoimmune diseases’ also on the list, this covers Hashimoto’s too.
So, both hypothyroidism and Hashimoto’s are considered to be risk factors, however, whether you are personally considered as ‘high risk’ will be decided on an individual basis.
Each pregnancy is different, including the mother-to-be and her personal health situation. What may be considered a risk to one woman, may not be for another.
With my first pregnancy, my NHS GP referred me to both an obstetrician and endocrinologist as he initially considered me to be ‘higher risk’, though not for my hypothyroidism or Hashimoto’s alone. The thyroid medication I was on, Armour Thyroid, (and subsequently took throughout pregnancy) was unfamiliar to him and much of the NHS. Unable to take the standard thyroid medication given on the NHS, Levothyroxine, I was on privately prescribed NDT medication; Armour Thyroid.
After seeing both the endocrinologist and obstetrician, I was discharged from both and any label of ‘possibly being high risk’ was withdrawn. They were happy with my private GP managing the thyroid medication dosage and didn’t see any reason to be more concerned with my pregnancy compared to another hypothyroid woman on Levothyroxine for example.
Related Articles:
10 “Truths” About My Pregnancies with Hypothyroidism and Hashimoto’s
Can I Prevent My Child From Developing Hashimoto’s or Hypothyroidism?
However, if you’re experiencing complications of your thyroid condition during pregnancy, e.g. levels fluctuating quite a lot or experiencing blood pressure concerns, then you may individually be considered as ‘high risk’. If you are also on a privately prescribed or self-sourced thyroid medication, or considered to be ‘borderline‘ hypothyroid and not on treatment, these may also play in to whether you’re labelled as ‘high risk’.
My second pregnancy was classed as high risk due to non-thyroid related complications. The doctors were not concerned about my medication this time either (I was on a combination of Armour and Levothyroxine for this pregnancy), but I had another complication which put myself and the baby at higher risk for issues.
It’s also worth noting that if you’re ‘borderline’ hypothyroid, your doctor may wish to start you on thyroid medication or increase it so that you’re well within range to reduce risk of miscarriage. The risk of miscarriage is higher in women with subclinical hypothyroidism, compared to women with normal thyroid function (euthyroidism). [2]
Subclinical hypothyroidism in the mother is also associated with a higher risk of pre-eclampsia. [3]
Generally, it seems that women on standard T4 thyroid medication such as Levothyroxine or Synthroid and are generally well and easily managed, are not considered to be ‘high risk’, but your doctor or healthcare team may have individual concerns about your particular situation.
Related Article: Were My Thyroid Pregnancies What I Expected?
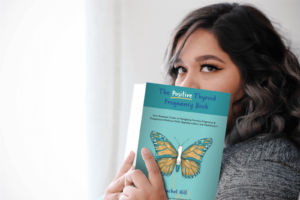
Don’t forget that The Positive Thyroid Pregnancy Book: Your Essential Guide to Navigating Fertility, Pregnancy & Postpartum Wellness With Hypothyroidism and Hashimoto’s also covers my two pregnancies with hypothyroidism and Hashimoto’s in a lot of detail, while also compiling ALL the info you need to know for the best start for you and your baby.
How To Keep Risks Low
As soon as you know you are pregnant, inform your doctor straight away and ensure a full thyroid panel blood test is conducted as soon as possible. That’s a full thyroid panel. Not just TSH and Free T4 – as Free T3 and thyroid antibodies are important too.
In the first trimester of pregnancy, the foetus relies completely on the mother to provide thyroid hormones for its development. For someone with a perfectly healthy thyroid gland and function, their body is able to meet that extra demand easily, but a woman with hypothyroidism may not be able to. So keep on top of your thyroid levels. Doctors often increase thyroid medication dosage as soon as a patient becomes pregnant and it is common practise to then retest levels every 4-6 weeks throughout pregnancy. Most women with existing hypothyroidism require an increase in thyroid medication when pregnant, to support the developing baby. [4]
Failure to properly maintain adequate thyroid levels whilst pregnant can result in complications such as miscarriage, pre-eclampsia, anaemia, stillbirth and the baby developing congenital hypothyroidism itself. [3], [5]
However, although women with thyroid issues are more likely to have obstetric complications than women without thyroid disease, it is important to know that most women with thyroid disease do not experience complications in pregnancy and in fact have a straightforward pregnancy and birth. Ensuring your thyroid levels are adequately managed is a key part of this.
Read about the 13 Things I Did in order to Have a Healthy Pregnancy With Hashimoto’s and Hypothyroidism here.
What has been your experience of pregnancy and hypothyroidism? Were you considered ‘high risk’?
You can click on the hyperlinks in the above post to learn more and see references to information given.
See Also:
The Positive Thyroid Pregnancy Book: Your Essential Guide to Navigating Fertility, Pregnancy & Postpartum Wellness With Hypothyroidism and Hashimoto’s which covers Rachel’s full two pregnancies with hypothyroidism and Hashimoto’s, on Levothyroxine and Armour Thyroid NDT and everything YOU need to know for the best start for you and your baby.
References:
[1] https://www.nichd.nih.gov/health/topics/high-risk/conditioninfo/factors
[2] https://www.ncbi.nlm.nih.gov/pubmed/31808375
[3] https://www.thelancet.com/journals/landia/article/PIIS2213-8587(22)00007-9/fulltext
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2533153/
[5] https://www.niddk.nih.gov/health-information/health-topics/endocrine/pregnancy-and-thyroid-disease/Pages/fact-sheet.aspx#pregnancy