What is it really like to go through pregnancy with hypothyroidism and Hashimoto’s?
I’ve been pregnant three times. The first ended in an early miscarriage, the second and third resulted in healthy, full-term babies. (for simplicity of this article, when I mention ‘my first pregnancy’ and ‘my second pregnancy’ I am referring to the two pregnancies which resulted in live births)
Many thyroid patients come to me anxious about pregnancy and unsure about whether they can have a healthy baby and also come out of pregnancy healthy themselves.
I already have various articles answering many of these frequently asked questions, such as:
- Do we need more thyroid medication in pregnancy?
- Are those with thyroid disease high risk?
- Are thyroid flare ups more frequent in pregnancy?
This post is going to delve in to my personal experiences with these frequently asked questions and topics. Did they apply to my pregnancies?
1. I Had a Lot of Extra Blood Tests
The question “Do we need more blood tests?” comes up often and yes, all doctors involved in my care whilst pregnant agreed that I needed regular, full thyroid panel blood tests. These included TSH, Free T3 and Free T4 every 4-6 weeks from the moment my pregnancy was confirmed until I gave birth.
Testing them this often meant that my thyroid levels were being closely monitored so that we could catch any need for medication dosage adjustments nice and early, keeping both myself and baby as well as possible.
It was my responsibility to remember to book in for my thyroid blood test every 4 weeks. I would have a reminder set in the calendar on my phone so that I knew when I needed to book in for another.
When not pregnant, my thyroid levels are tested every 6 months, so going from this to once a month was definitely a big increase in the amount of blood draws!
My midwife also decided to run other regular tests too, including those for diabetes, liver function and vitamin levels such as ferritin and Vitamin D, due to my thyroid condition. On average, I was having blood tests every couple of weeks all the way through my pregnancies.
2. I Was ‘High Risk’
Not all pregnant people with a thyroid condition will automatically be classed as high risk. It is decided on a patient by patient basis and factors such as which type of thyroid medication you are on, how well controlled your thyroid condition is and whether you have other risk factors (such as obesity, high blood pressure, or other health conditions too) will impact this.
Each pregnancy is different, including the mother-to-be and her personal health situation. What may be considered a risk to one woman, may not be for another.
With my first pregnancy, my NHS GP referred me to both an obstetrician and endocrinologist as he initially considered me to be ‘higher risk’, though not for my hypothyroidism or Hashimoto’s alone. The thyroid medication I was on, Armour Thyroid, (and subsequently took throughout the pregnancy) was unfamiliar to him and much of the NHS, so he considered this to be a risk factor.
After seeing both an endocrinologist and obstetrician, I was discharged by them and any label of ‘possibly being high risk’ was withdrawn. They were happy with my private GP managing the thyroid medication and didn’t see any reason to be more concerned with my pregnancy compared to another hypothyroid woman on the standard treatment of Levothyroxine for example.
My second pregnancy was classed as high risk due to non-thyroid related complications. The doctors were not concerned about my medication this time around (I was on a combination of Armour and Levothyroxine for my second pregnancy), but I had another, non-thyroid complication which put myself and the baby at higher risk for other issues. They weren’t concerned about my thyroid condition at all during the second pregnancy.
3. I Felt Better While Pregnant
Minus the typical pregnancy symptoms of fatigue, sickness and aches and pains, I did feel better while pregnant in terms of my thyroid condition. I experienced less flares, my Hashimoto’s stayed in remission and undetectable for both pregnancies, and my thyroid symptoms were non-existent as long as my thyroid levels were kept in the optimal range (which is why testing them so often was important!)
Thyroid symptoms I had previous to pregnancy, such as acne and migraines disappeared while pregnant.
4. I Didn’t Have as Many Flares as I Expected
As touched on in the previous point, I didn’t experience many thyroid flares at all, during both pregnancies, which really surprised me.
Prior to ever falling pregnant, I would look ahead and feel anxious about the idea of having a lot of ‘tough thyroid days’ when pregnant one day. So to not have this be the case at all was a real surprise (and bonus).
Hormonal fluctuations such as pregnancy are an unsurprising flare trigger, as well as the amount of extra work pregnancy is demanding from your body. Whilst I did still experience some, I definitely didn’t experience a lot.
The flares I did have were mostly limited to the first trimester, which is always the hardest in terms of fatigue and symptoms anyway, and they would last just a day. I luckily didn’t have day after day of flares.
Overall, my thyroid condition was very well managed in my first pregnancy, though less well managed in my second, as during the first 20 weeks of the second, my levels bounced around a lot and it took some time to get my thyroid medication dosage correct. Even so, I didn’t experience a sharp increase in thyroid flares, just overall more thyroid symptoms creeping back in.
5. I Was Consultant Led
As touched on in point number 3, I was initially consultant led in the first pregnancy, by an endocrinologist and obstetrician, who both ultimately discharged me early on in the pregnancy.
For my second pregnancy I was consultant led all the way through, though not for my thyroid condition but for non-thyroid related complications which developed later on.
6. My Thyroid Meds Only Needed Increasing Towards the End
This is true for my first pregnancy. I was on Armour Thyroid for the first, which remained constant and kept my thyroid levels optimal right until the last two months of pregnancy. It surprised us all, since most need a medication dosage alteration before this! It was increased by just 15% for the last two months.
In my second pregnancy, the Armour Thyroid still did not need adjusting until right towards the end, but the Levothyroxine I was also on alongside it was different. This was adjusted three times during the first 20 weeks alone.
7. Doctors Didn’t Approve of My Type of Thyroid Medication
Entering in to my first pregnancy on Armour Thyroid, a medication I knew the NHS wouldn’t approve of, was nerve wracking. However, I was adamant to stay on it because I knew it was what was best for myself and my growing baby.
I wasn’t surprised when it was met with pushback and an endocrinologist who tried her best to convince me to switch back to Levothyroxine.
8. I Had to Keep Adjusting My Supplements
As soon as I knew I was pregnant, I checked which of my supplements were safe to continue. We did this by retesting key vitamin levels such as a full iron panel, B12 and Vitamin D, in order to determine what adjustments to supplements were needed.
I took a good prenatal throughout pregnancy, as recommended by the GP and midwife, whilst also supplementing some extras on top (determined by blood tests and my personal requirements) such as Vitamin C, Selenium, Vitamin D, Vitamin K, iron and magnesium. I also took a probiotic throughout both pregnancies.
I revisited supplements throughout my pregnancies, retesting levels and adjusting where needed every couple of months. Increasing the magnesium supplementation slightly helped with leg cramping and mild constipation.
9. I Had to Change My Exercise
Prior to my first pregnancy, I took long walks everyday, did two 1-hour aerobic dance classes per week and 1-2 salsa dance classes per week.
By the time I was in the second trimester of my first pregnancy, I found that I couldn’t safely keep up with this level of exercise anymore. I was feeling lightheaded and therefore needed to reassess.
I started an antenatal yoga class at 13 weeks, both times, kept up walks throughout both pregnancies and began swimming, too.
Walking, swimming and yoga worked really well for me. I still got a good work out (especially from swimming) but didn’t feel completely wiped out. It can feel frustrating to have to change your exercise routines, especially if you have a form of movement you really love, but I decided to embrace the changes my body needed.
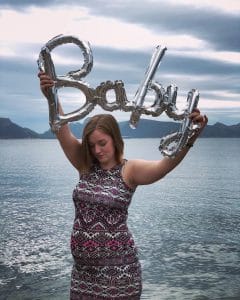
10. My Babies Were Healthy
Thankfully, my two baby boys arrived healthy and without any issues. Looking back now at the Rachel who was so very anxious at the thought of having children because she wasn’t sure if she’d be able to have them or get through pregnancy with all the thyroid luggage, I want to reassure her that it can be done.
Yes, having hypothyroidism and / or Hashimoto’s does indeed increase the chances of pregnancy loss and other complications, however, much of this can be avoided with correct monitoring and management. I do feel incredibly lucky for my children and I appreciate that not everyone has the same experience.
However, I want to reassure others who feel anxious about the prospect of starting a family, and tell them that it is possible to reach this happy outcome. I hope my posts help with this.
You’re welcome to add your own experiences in the comments section below.
Related Posts:
Were My Thyroid Pregnancies What I Expected?
5 Tips For a Healthy Thyroid Pregnancy
11 Things I Did to Optimise Conceiving With Hashimoto’s and Hypothyroidism
 See also:
See also:
You, Me and Hypothyroidism: When Someone You Love Has Hypothyroidism, a book for those who know someone with hypothyroidism. It looks at how pregnancy, fertility, parenting, home life and more can all be affected by hypothyroidism, and what you can do about it.







 See also:
See also: